Preserving Vision with Eye Disease Management in Garfield County
Through a combination of advanced diagnostic techniques, comprehensive treatment plans, and co-management with specialists, we strive to preserve vision by addressing eye diseases in their earliest stages.
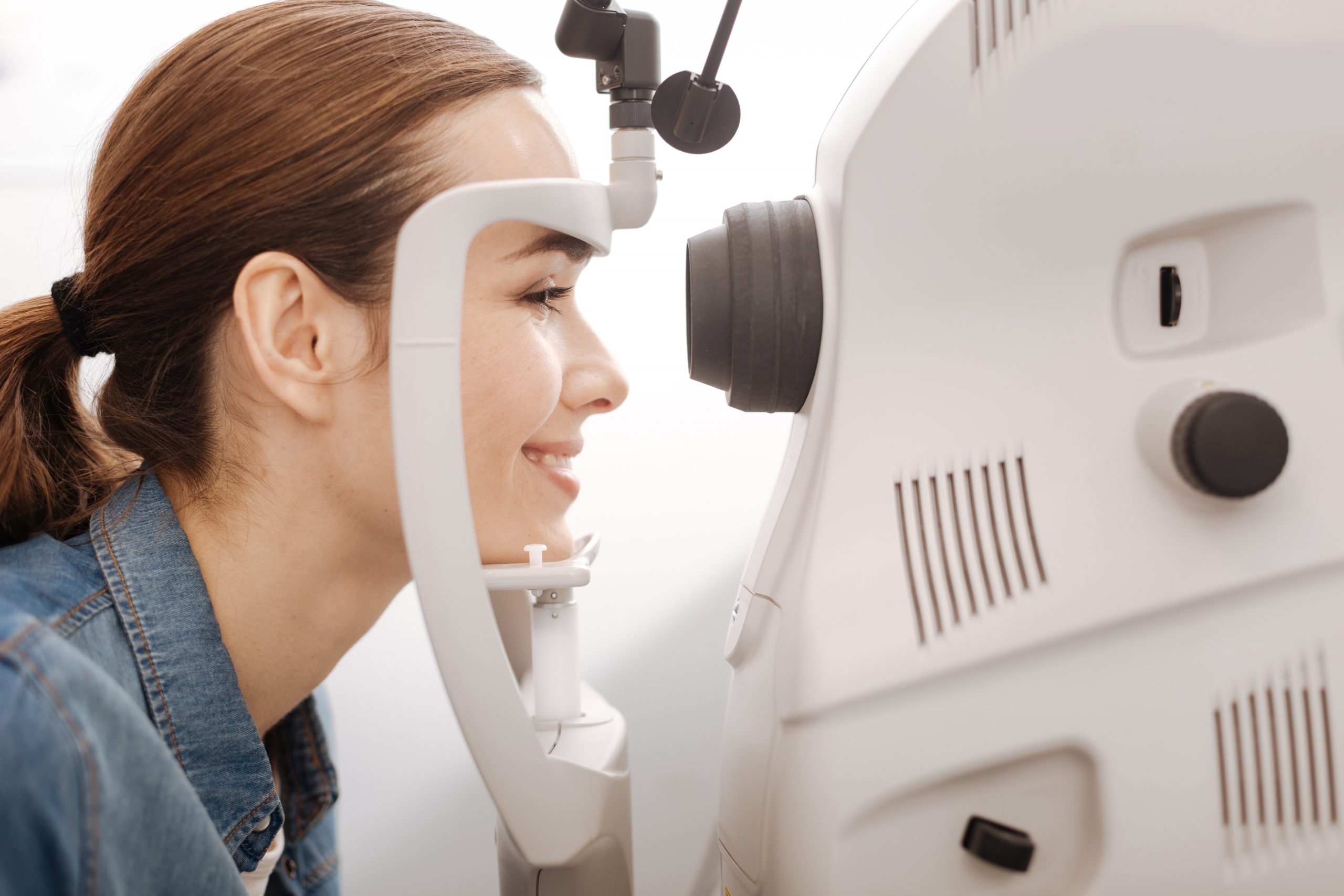
Eye Diseases We’ll Help You Manage at 20/20 Eyecare

Glaucoma: Types and Warning Signs
Glaucoma is a group of eye diseases that damages the eye's optic nerve and tends to worsen over time. The two most common forms of the disease are open-angle glaucoma and angle-closure glaucoma. Open-angle glaucoma is less severe and often presents no noticeable symptoms until irreversible damage has occurred. Signs of angle-closure glaucoma include blurry or hazy vision, eye redness, nausea and vomiting, severe eye or forehead pain, and seeing rainbows or halos. Seek emergency medical care if you experience any of those symptoms.
Expert Care for Macular Degeneration: Slowing Progression
As leading macular degeneration eye doctors, we provide advanced care for patients facing this challenging condition. Our focus is on slowing the rate at which the macula deteriorates through a combination of lifestyle adjustments, nutritional guidance, and appropriate medical treatments. Surgery may be necessary in certain advanced cases. In that case, our optometrists can refer you to qualified ophthalmologists for the specialized surgical care you need.


Seamless Cataract Support
Cataract co-management is a vital service we offer to ensure that patients in Glenwood Springs and Carbondale receive comprehensive support before, during, and after cataract surgery. Our eye care team works closely with ophthalmologists to prepare you for the procedure, providing detailed exams and guidance on what to expect. Post-surgery, we continue to monitor your recovery, adjust your vision correction as needed, and manage any possible complications.
Managing Diabetic Retinopathy: Early Detection and Treatment
Diabetic retinopathy is an eye disease caused by unmanaged diabetes. It damages the blood vessels in the retina and can lead to permanent vision loss. Our comprehensive screening services detect changes in the retina at the earliest possible stage, allowing us to respond with appropriate treatments that preserve your vision. Additionally, our team provides education on managing diabetes to protect your eye health and liaises with your diabetic physician to keep the condition under control.
Call 20/20 Eyecare to request your eye exam today!

